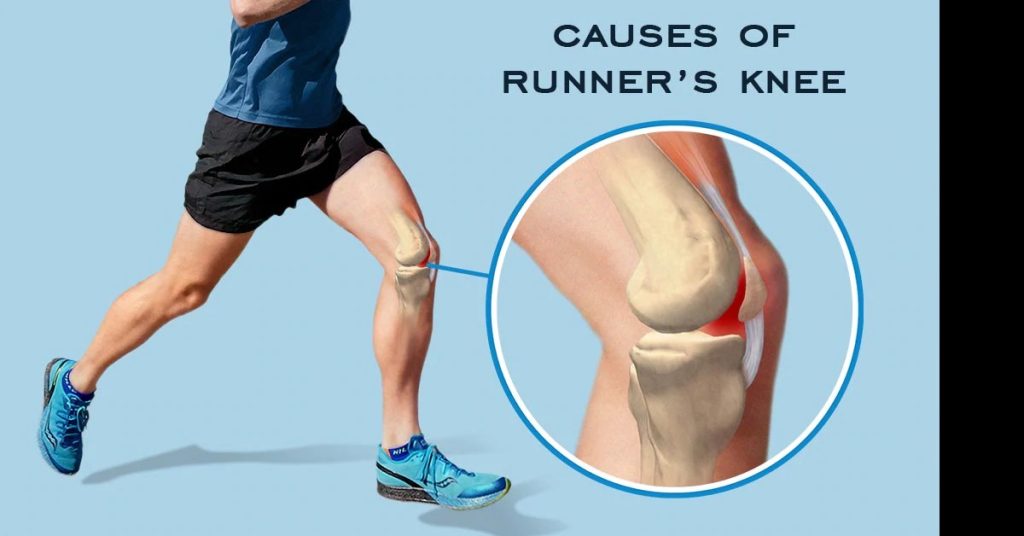
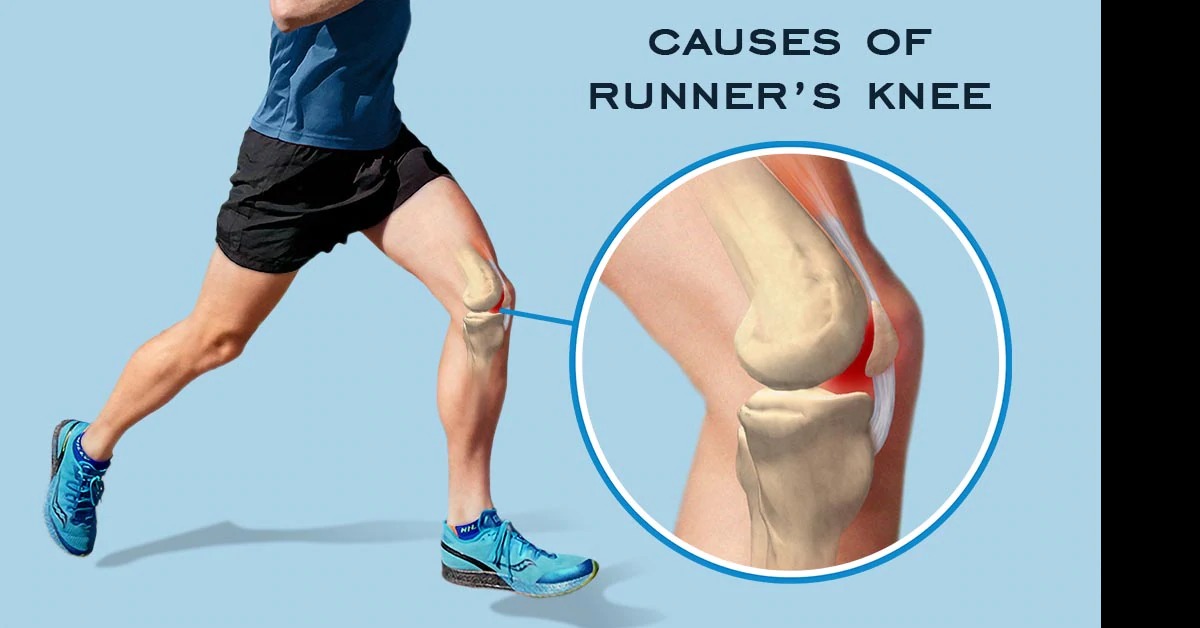
Experiencing knee pain when running? You’re not alone. Runner’s knee, medically known as patellofemoral pain syndrome (PFPS), affects up to 25% of all runners and is one of the most common running injuries. Whether you’re dealing with a dull ache around your kneecap or sharp pain that stops you mid-run, understanding the causes, treatment options, and prevention strategies is crucial for getting back to pain-free running.
This comprehensive guide provides evidence-based information on runner’s knee, helping you identify symptoms, understand treatment options, and implement proven prevention strategies to keep you running strong.
Important Medical Disclaimer: This article is for educational purposes only and should not replace professional medical advice. Always consult with a healthcare provider for proper diagnosis and treatment of knee pain.
What is Runner’s Knee?
Runner’s knee (patellofemoral pain syndrome) is a broad term describing pain around or behind the kneecap (patella) where it connects with the thigh bone (femur). Despite its name, runner’s knee doesn’t exclusively affect runners—it’s common among cyclists, hikers, jumpers, and anyone who participates in activities involving repetitive knee bending.
Key Characteristics:
- Pain location: Around or behind the kneecap
- Pain pattern: Often worse with activity, stairs, or prolonged sitting
- Prevalence: Affects 25% of runners annually
- Demographics: More common in women (2:1 ratio) and younger athletes
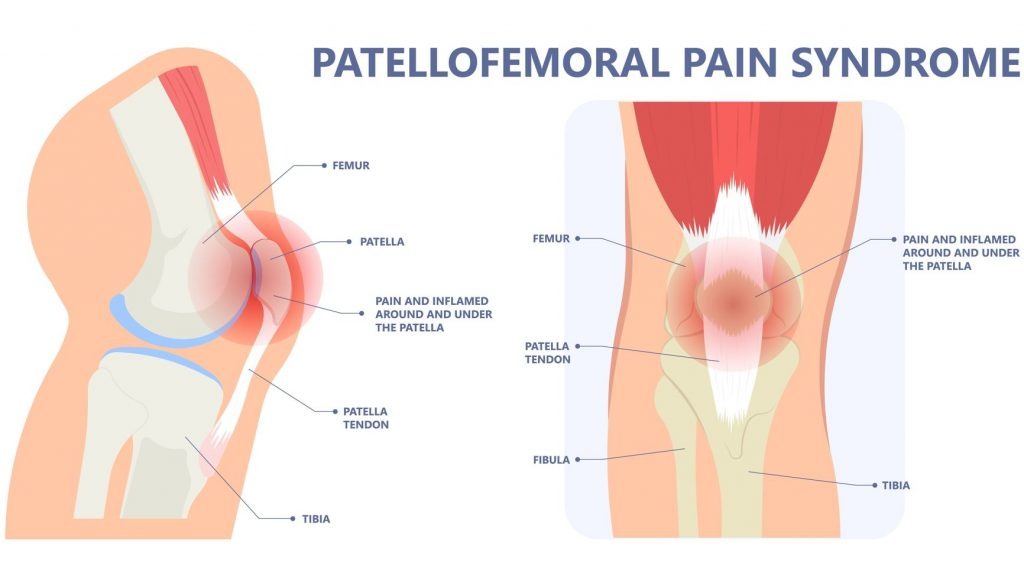
Understanding Knee Anatomy
To effectively address runner’s knee, it’s essential to understand the complex structure of your knee joint:
Primary Knee Components:
Bones:
- Femur (thigh bone): Upper leg bone
- Tibia (shin bone): Larger lower leg bone
- Patella (kneecap): Triangular bone protecting the knee joint
Cartilage:
- Articular cartilage: Smooth surface covering bone ends
- Meniscus: C-shaped cartilage cushioning tibia and femur
Supporting Structures:
- Quadriceps muscles: Four muscles controlling knee extension
- Patellar tendon: Connects patella to tibia
- Ligaments: Provide stability (ACL, PCL, MCL, LCL)
- IT band: Fibrous tissue running along outer thigh
How Runner’s Knee Develops:
The patella sits in a groove (trochlea) on the end of the femur. During running, the patella must track smoothly within this groove as the knee bends and straightens. When biomechanical factors cause the patella to maltrack, it creates:
- Increased pressure on cartilage surfaces
- Inflammation of surrounding tissues
- Pain during weight-bearing activities
Runner’s Knee Symptoms and Recognition
Primary Symptoms:
Pain Characteristics:
- Dull ache around or behind the kneecap
- Sharp pain during running, especially downhill
- Tenderness when touching the kneecap
- Pain with stairs: Particularly going downstairs
- Stiffness after prolonged sitting (“theater sign”)
Associated Symptoms:
- Grinding sensation (crepitus) when bending the knee
- Swelling around the kneecap
- Feeling of instability or “giving way”
- Popping sounds during knee movement
Symptom Severity Scale:
Mild (Grade 1):
- Pain only after running
- No pain during daily activities
- Able to continue training with modifications
Moderate (Grade 2):
- Pain during running that doesn’t stop activity
- Occasional pain during daily activities
- May need to reduce training intensity
Severe (Grade 3):
- Pain that stops running activity
- Significant pain during daily activities
- Unable to run without severe discomfort
Common Causes of Runner’s Knee
Understanding the root causes of runner’s knee is essential for effective treatment and prevention:
Biomechanical Factors:
1. Overuse and Training Errors
- Sudden increase in mileage or intensity (>10% weekly)
- Excessive downhill running increasing patella stress
- Inadequate recovery between training sessions
- Poor progression in training programs
2. Muscle Imbalances and Weakness
- Weak quadriceps: Particularly the vastus medialis oblique (VMO)
- Tight hip flexors: Alter patellar tracking mechanics
- Weak glutes: Lead to excessive hip adduction and knee valgus
- Calf tightness: Changes running mechanics and load distribution
3. Anatomical and Structural Issues
- Patellar malalignment: Naturally higher Q-angle (especially in women)
- Flat feet (overpronation): Excessive inward foot rolling
- High arches: Reduced shock absorption
- Leg length discrepancy: Asymmetrical loading patterns
Environmental and Equipment Factors:
Running Surface Issues:
- Hard surfaces: Concrete and asphalt increase impact forces
- Cambered roads: Create asymmetrical loading
- Steep downhills: Dramatically increase patellofemoral stress
- Uneven terrain: Requires constant adaptation
Footwear Problems:
- Worn-out shoes: Loss of cushioning and support after 300-500 miles
- Incorrect shoe type: Wrong category for foot type or gait pattern
- Poor fit: Too small, too large, or inappropriate width
- Inadequate support: Insufficient arch support or motion control
Differential Diagnosis: Other Knee Conditions
It’s important to distinguish runner’s knee from other knee problems that cause similar symptoms:
IT Band Syndrome:
- Pain location: Outer knee and thigh
- Pain pattern: Sharp pain along IT band
- Tenderness: Over lateral femoral condyle
Meniscus Tears:
- Pain location: Joint line (inner or outer knee)
- Mechanism: Often sudden onset with twisting
- Symptoms: Locking, catching, or limited range of motion
Patellar Tendinitis:
- Pain location: Below the kneecap at patellar tendon
- Pain pattern: Sharp, localized pain with jumping/landing
- Tenderness: Directly over patellar tendon
Chondromalacia Patella:
- Definition: Actual cartilage damage under the patella
- Relationship: Can be a progression of untreated runner’s knee
- Diagnosis: Requires imaging (MRI) for confirmation
Evidence-Based Treatment Strategies
Effective runner’s knee treatment follows a multi-faceted approach addressing both symptoms and underlying causes:
Phase 1: Acute Management (0-2 weeks)
Immediate Care Protocol:
- Relative rest: Reduce or temporarily cease running
- Ice application: 15-20 minutes every 2-3 hours for first 48-72 hours
- Compression: Elastic bandage or patellar strap during activities
- Elevation: Elevate leg when resting to reduce swelling
Activity Modification:
- Avoid aggravating activities: Stairs, squats, prolonged sitting
- Cross-training options: Swimming, cycling (if pain-free), upper body exercises
- Pain monitoring: Use 0-10 pain scale to guide activity levels
Phase 2: Rehabilitation and Strengthening (2-8 weeks)
Quadriceps Strengthening Program:
Week 1-2: Basic Strengthening
- Quadriceps sets: 3 sets of 15 reps, hold 5 seconds
- Straight leg raises: 3 sets of 15 reps each direction
- Wall sits: 3 sets, progress from 15-60 seconds
- Step-ups: 4-6 inch step, 2 sets of 10 reps
Week 3-4: Progressive Loading
- Single-leg squats: 3 sets of 8-12 reps (partial range)
- Lateral lunges: 3 sets of 10 reps each leg
- Clamshells: 3 sets of 15 reps for hip stability
- Bridges: Progress to single-leg bridges, 3 sets of 10
Week 5-8: Functional Exercises
- Plyometric step-ups: 3 sets of 8-10 reps
- Single-leg deadlifts: 3 sets of 8-10 reps
- Lateral step-downs: 3 sets of 10 reps (controlled)
- Jump squats: 3 sets of 8-10 reps (if pain-free)
Flexibility and Mobility Program:
Daily Stretching Routine:
- Quadriceps stretch: Hold 30 seconds x 3 reps
- Hip flexor stretch: Hold 30 seconds x 3 reps each leg
- IT band stretch: Hold 30 seconds x 3 reps each leg
- Calf stretch: Hold 30 seconds x 3 reps each leg
- Hamstring stretch: Hold 30 seconds x 3 reps each leg
Foam Rolling Protocol:
- Quadriceps: 60-90 seconds daily
- IT band: 60-90 seconds daily (avoid rolling directly on knee)
- Calves: 60-90 seconds daily
- Glutes: 60-90 seconds daily
Phase 3: Return to Running (6-12 weeks)
Graduated Running Program:
Week 1-2: Walk-Run Intervals
- Day 1: Walk 2 min, run 1 min x 6 cycles
- Day 2: Rest or cross-train
- Day 3: Walk 90 sec, run 90 sec x 6 cycles
- Progress: Only if pain-free during and after activity
Week 3-4: Continuous Running
- Day 1: 15-minute continuous run
- Day 2: Rest or easy cross-training
- Day 3: 20-minute continuous run
- Day 4: Rest
- Day 5: 25-minute continuous run
Week 5+: Normal Training Resumption
- Gradual mileage increase: Follow 10% rule
- Surface variety: Prioritize softer surfaces initially
- Pain monitoring: Stop if pain exceeds 3/10 during activity
Professional Treatment Options
When to Seek Medical Care:
Immediate Medical Attention Required:
- Sudden, severe pain with inability to bear weight
- Obvious deformity or instability
- Locking sensation preventing knee movement
- Significant swelling within hours of injury
Consult Healthcare Provider If:
- Pain persists beyond 2-3 weeks of conservative treatment
- Pain interferes with daily activities
- Recurrent episodes despite prevention efforts
- Numbness or tingling around the knee
Medical Treatment Options:
Physical Therapy:
- Professional assessment: Comprehensive biomechanical evaluation
- Manual therapy: Joint mobilization and soft tissue techniques
- Exercise prescription: Customized strengthening and flexibility programs
- Movement retraining: Gait analysis and correction
Medical Interventions:
- Anti-inflammatory medications: NSAIDs for pain and inflammation control
- Corticosteroid injections: For severe, persistent inflammation
- Platelet-rich plasma (PRP): Emerging treatment for cartilage healing
- Patellar taping/bracing: Biomechanical support during activity
Advanced Imaging:
- X-rays: Rule out fractures or bone abnormalities
- MRI: Detailed soft tissue evaluation for cartilage, ligaments, meniscus
- CT scan: Detailed bone structure assessment
Surgical Options (Rare):
- Arthroscopic surgery: Cartilage cleanup or realignment procedures
- Lateral release: Release tight lateral structures
- Tibial tubercle transfer: Realignment of patellar tracking
Prevention Strategies: Keeping Runner’s Knee at Bay
Prevention is always better than treatment. Implement these evidence-based strategies to reduce your risk of developing runner’s knee:
Training Modifications:
Smart Progression Protocol:
- 10% rule: Increase weekly mileage by no more than 10%
- Periodization: Include easier weeks every 3-4 weeks
- Surface variety: Mix soft trails, tracks, and harder surfaces
- Downhill limits: Limit steep downhill training, especially early in programs
Cross-Training Integration:
- Strength training: 2-3 sessions per week focusing on legs and core
- Low-impact cardio: Swimming, cycling, elliptical on non-running days
- Flexibility work: Daily stretching routine focusing on major muscle groups
- Recovery activities: Yoga, easy walking, foam rolling
Biomechanical Optimization:
Running Form Improvement:
- Cadence: Aim for 180+ steps per minute to reduce impact forces
- Foot strike: Midfoot landing rather than heel striking
- Posture: Slight forward lean from ankles, not waist
- Arm swing: Relaxed, efficient arm movement
Muscle Balance Maintenance:
- Weekly strength training: Focus on quadriceps, glutes, and core
- Hip stability work: Single-leg exercises and lateral movements
- Posterior chain strengthening: Hamstrings and glutes for balance
- Core stability: Planks, side planks, and rotational exercises
Equipment and Footwear:
Proper Running Shoes:
- Regular replacement: Every 300-500 miles or when tread worn
- Appropriate type: Match shoe category to foot type and gait pattern
- Professional fitting: Get gait analyzed and properly fitted
- Gradual transition: When changing shoe types or brands
For comprehensive reviews and expert recommendations on running shoes specifically designed for runners with knee pain, including motion control and stability features that can help prevent runner’s knee, visit shoeexpert.net. Their detailed guides help you select footwear with proper support, cushioning, and biomechanical features to reduce knee stress and prevent injury recurrence.
Additional Equipment:
- Orthotics: Custom or over-the-counter arch supports if needed
- Patellar straps: May provide symptomatic relief during activity
- Compression sleeves: Can help with proprioception and support
- Proper clothing: Moisture-wicking fabrics and appropriate layering
Lifestyle Factors:
Weight Management:
- Healthy body weight: Each pound of excess weight adds 4 pounds of stress to knees
- Balanced nutrition: Support tissue repair and reduce inflammation
- Hydration: Maintain proper fluid balance for joint lubrication
Recovery Optimization:
- Adequate sleep: 7-9 hours nightly for tissue repair
- Stress management: Chronic stress impairs healing and increases injury risk
- Nutrition timing: Post-workout nutrition within 30 minutes for optimal recovery
Recovery Timeline and Expectations
Understanding realistic recovery timelines helps set appropriate expectations and prevents premature return to full activity:
Typical Recovery Phases:
Mild Runner’s Knee (Grade 1): 2-4 weeks
- Week 1-2: Focus on relative rest and symptom management
- Week 3-4: Gradual return to running with modifications
- Full return: Usually possible within 4 weeks with proper management
Moderate Runner’s Knee (Grade 2): 4-8 weeks
- Week 1-3: Aggressive conservative treatment and strengthening
- Week 4-6: Progressive loading and activity modification
- Week 7-8: Gradual return to full training
- Full return: 6-8 weeks with comprehensive rehabilitation
Severe Runner’s Knee (Grade 3): 8-16+ weeks
- Week 1-4: Comprehensive rest and professional treatment
- Week 5-8: Intensive rehabilitation and biomechanical correction
- Week 9-12: Gradual activity progression with monitoring
- Week 13+: Return to full activity with ongoing prevention strategies
Factors Affecting Recovery:
Positive Prognostic Factors:
- Early intervention and proper diagnosis
- Good compliance with treatment program
- Absence of structural abnormalities
- Strong social support and motivation
Negative Prognostic Factors:
- Delayed treatment or continued running through pain
- Multiple contributing biomechanical factors
- Previous episodes of runner’s knee
- Concurrent injuries or health conditions
Nutrition for Knee Health and Recovery
Proper nutrition plays a crucial role in both recovery from runner’s knee and long-term joint health:
Anti-Inflammatory Foods:
Omega-3 Rich Options:
- Fatty fish: Salmon, mackerel, sardines (2-3 servings weekly)
- Plant sources: Walnuts, chia seeds, flax seeds (daily portions)
- Supplements: Fish oil or algae-based omega-3s if dietary intake inadequate
Antioxidant-Rich Foods:
- Colorful vegetables: Bell peppers, leafy greens, purple cabbage
- Berries: Blueberries, cherries, strawberries for anthocyanins
- Spices: Turmeric, ginger for natural anti-inflammatory compounds
Joint-Supporting Nutrients:
Collagen Building Blocks:
- Vitamin C: Citrus fruits, bell peppers, strawberries
- Protein: Complete proteins providing all essential amino acids
- Glycine: Found in bone broth, gelatin supplements
Cartilage Health:
- Glucosamine/Chondroitin: May support cartilage maintenance
- MSM (Methylsulfonylmethane): Potential anti-inflammatory benefits
- Vitamin D: Essential for bone health and muscle function
Hydration Strategy:
Daily Fluid Intake:
- Base needs: 35-40ml per kg body weight daily
- Exercise additions: 500-750ml per hour of activity
- Post-exercise: 150% of fluid lost through sweat
Mental Health and Injury Management
Dealing with runner’s knee involves more than just physical treatment—the mental and emotional aspects are equally important:
Psychological Impact:
Common Emotional Responses:
- Frustration: Inability to run as desired
- Anxiety: Fear of re-injury or permanent damage
- Depression: Loss of primary coping mechanism or social activity
- Identity crisis: For runners who define themselves through the sport
Coping Strategies:
Positive Mindset Development:
- Focus on controllables: Rehabilitation exercises, nutrition, sleep
- Set process goals: Rather than just outcome-based targets
- Celebrate small wins: Progress in strength, flexibility, or pain reduction
- Maintain perspective: View injury as opportunity for improvement
Social Support:
- Stay connected: With running community even if not actively running
- Communicate needs: Let friends and family know how they can help
- Professional support: Consider counseling if mental health significantly affected
Alternative Activities:
- Cross-training variety: Try new activities to maintain fitness and enjoyment
- Skill development: Use time for strength training, flexibility, or technique work
- Goal redirection: Set goals in other areas of life or different sports
Special Considerations
Women and Runner’s Knee:
Higher Risk Factors:
- Anatomical differences: Wider pelvis creating larger Q-angle
- Hormonal influences: Estrogen effects on ligament laxity
- Muscle activation patterns: Different quadriceps firing patterns
Targeted Interventions:
- Enhanced hip strengthening: Focus on glute medius and maximus
- Core stability training: Address potential strength differences
- Movement training: Emphasis on proper landing mechanics
Age-Related Considerations:
Younger Athletes (Under 18):
- Growth considerations: Account for rapid changes in height/weight
- Activity modification: May need sport-specific restrictions
- Professional guidance: Early intervention to prevent long-term issues
Older Runners (Over 40):
- Degenerative changes: May have underlying cartilage wear
- Recovery time: Generally longer healing periods required
- Comorbidities: Consider other health conditions affecting recovery
Return to Competition:
Readiness Criteria:
- Pain-free activity: No pain during running at planned race pace
- Strength requirements: 90% strength of uninjured leg
- Functional tests: Able to complete sport-specific movements without compensation
- Psychological readiness: Confidence in ability to perform without re-injury
Frequently Asked Questions
Q: Can I continue running with mild runner’s knee pain? A: Generally not recommended. Continuing to run through pain often worsens the condition and prolongs recovery. It’s better to take 2-3 weeks of modified activity than risk months of more severe problems.
Q: How long does runner’s knee take to heal? A: Recovery time varies based on severity and individual factors. Mild cases may resolve in 2-4 weeks with proper treatment, while severe cases can take 8-16 weeks or longer.
Q: Will runner’s knee come back once I’ve had it? A: Runner’s knee can recur, especially if underlying biomechanical issues aren’t addressed. However, proper rehabilitation, strength maintenance, and training modifications significantly reduce recurrence risk.
Q: Is it safe to use anti-inflammatory medications for runner’s knee? A: NSAIDs can be helpful for short-term pain and inflammation control but should be used judiciously due to potential side effects. Consult with a healthcare provider for appropriate use and duration.
Q: Should I get an MRI for runner’s knee? A: MRI is typically not necessary for uncomplicated runner’s knee. It may be recommended if conservative treatment fails after 6-8 weeks or if other conditions are suspected.
Q: Can orthotics help with runner’s knee? A: Custom or over-the-counter orthotics can be beneficial if foot mechanics contribute to knee pain. A professional assessment can determine if orthotics would be helpful in your specific case.
Q: What’s the difference between runner’s knee and IT band syndrome? A: Runner’s knee causes pain around/behind the kneecap, while IT band syndrome typically causes pain on the outer side of the knee. The treatments and underlying causes can be different.
Q: Can I prevent runner’s knee if I’ve never had it? A: Yes! Proper training progression, strength maintenance, appropriate footwear, and good running mechanics significantly reduce your risk of developing runner’s knee.
Conclusion: Your Path to Pain-Free Running
Runner’s knee is a common but highly treatable condition that affects millions of runners worldwide. With proper understanding, early intervention, and comprehensive management, most runners can return to pain-free activity and reduce their risk of recurrence.
Key Takeaways for Runner’s Knee Management:
Early Recognition and Action:
- Don’t ignore persistent knee pain—early intervention leads to better outcomes
- Seek professional help if pain persists beyond 2-3 weeks of conservative treatment
- Understand that temporary activity modification prevents long-term problems
Comprehensive Treatment Approach:
- Address both symptoms and underlying biomechanical causes
- Combine rest, strengthening, flexibility work, and gradual return to activity
- Consider professional guidance for complex or persistent cases
Prevention is Paramount:
- Maintain strength and flexibility through regular training
- Follow proper training progression and recovery principles
- Invest in appropriate footwear and replace shoes regularly
- Address biomechanical issues before they become problems
Long-term Success Strategies:
- Develop a sustainable training approach that includes variety and recovery
- Maintain strength training and flexibility work throughout your running career
- Listen to your body and adjust training based on how you feel
- Build a support network of healthcare professionals and fellow runners
Remember, runner’s knee doesn’t have to end your running career. With patience, proper treatment, and smart prevention strategies, you can overcome this common injury and return to the activity you love. The key is taking action early, being consistent with treatment, and addressing the underlying factors that contributed to the problem in the first place.
Your journey back to pain-free running starts with understanding your condition and committing to a comprehensive approach to treatment and prevention. Stay patient, stay consistent, and don’t hesitate to seek professional help when needed.